Simplified Approach through Physician Alignment and Integration
Value Based Care is defined as provision of services that are low cost, highly efficient, service-oriented and provide the highest quality outcomes. Consumer expectations of values in the healthcare industry will continue to increase. Serving healthcare needs of a community that meet and exceed consumer expectations is complex and multi-faceted. The healthcare industry needs a simplified approach to address complexity and move toward a coordinated care delivery system. Healthcare organizations must first define a compelling vision for coordinated care delivery. Execution of that vision is best achieved through a leadership philosophy of performance excellence.
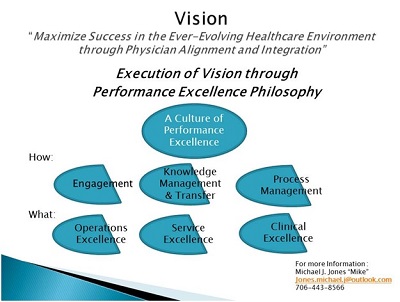
The schematic shown below provides a roadmap for navigating the performance excellence journey toward value-based care (see schematic). This introductory article, the first in a series, outlines a vision for maximizing organizational success in the evolving healthcare industry through physician alignment and integration. A consistent and simplified leadership philosophy is provided to assist in execution of a strategic vision. Organizational gaps that may interfere with achieving organizational vision are also identified.
Vision and Execution:
The journey begins with:

- Strategic vision for the future, and
- Execution of the strategic vision through a leadership philosophy and organization culture of performance excellence.
The culture of performance excellence focuses on measurable results and outcomes in three main areas:
- Operating/Financial Excellence,
- Service Excellence, and
- Clinical Excellence.
Performance excellence is best achieved when time and energy are devoted to:
- Key Stakeholder Engagement,
- Knowledge Management/Knowledge Transfer through data analytics, and
- Formal Process Management.
Organizational Gaps:

Physicians and other providers are often not fully aligned with hospital organizations. Competing interests among physicians, other providers and hospital organizations may exacerbate misalignment. Hospital organizations know they need physician alignment and integration strategies. Many hospital organizations are unclear regarding scope of physician alignment and integration strategies. Some hospital organizations tend to view integration as a model of employment only, when there is a vast array of physician integration models.
Each hospital organization possesses a unique climate and organizational culture for effective physician integration. Execution of physician integration strategies may lack depth of understanding. Structure and infrastructure needs for effective strategy execution are often underestimated. Governance, Leadership and Management representation among physicians and other providers is necessary, but often ignored. Significant variation in level of engagement exists among key stakeholders in healthcare delivery. High levels of engagement in organizational change are needed among leadership, management, physicians, other providers and staff, as key stakeholders in the delivery of care. Common understanding among key stakeholders is often lacking.
Traditional healthcare leaders may have a tendency to exert “control” rather than engage physicians and other providers when focusing on organizational initiatives to improve care delivery. In addition, development of multi-disciplinary teams to focus on organizational initiatives may be difficult. Multi-disciplinary teams are especially prone to experiencing team dynamics of forming, storming, norming and performing. Many organizations have a low tolerance for the highly productive storming phase of team development, especially when physicians are involved. Embracing physician input is imperative.
Many healthcare organizations have not adopted a meaningful and comprehensive process management methodology. There may be tendency to focus process management efforts within the confines of the hospital organization. Process management initiatives must become much broader in scope, must address care delivery across the entire continuum of care, and must focus on enterprise-wide initiatives, including care delivery in physician offices. Application of a formal and reliable process management methodology is often underestimated. Establishing an enterprise-wide process management approach requires vision, and investment of time and money. Physician stakeholders, being scientifically trained, tend to naturally adopt process management principles. The investment in education and training may be substantial. A multitude of models exist and it may be difficult to select and sustain a consistent approach that is embraced by all key stakeholders.
There exists an ever-increasing emphasis on service, cost and quality outcomes. Government payers are increasing regulatory requirements, but those requirements may not be universally understood. Variation in understanding among key stakeholders may exist. Non-governmental payers may institute additional requirements and variation adds complexity and lack of common understanding. Employer demand for reduced healthcare costs, while providing service oriented and quality services, creates another set of demands on healthcare providers. Suppliers and vendors to the healthcare industry lack a comprehensive view of what is needed to improve service delivery.
Traditional hospital based healthcare organizations are deeply grounded in meeting the needs of the communities in which they serve. Traditionally, hospital based organizations have long and established histories of serving patients at times when they are most in need of life saving intervention. Consumers and payers of the healthcare industry expect an effort to create healthier communities and to reduce high cost, episodic and acute interventions. Healthcare systems are not always well positioned to meet comprehensive consumer expectations beyond episodes of care. Healthcare systems have traditionally survived and measured success, based on payment models that encourage utilization of high cost, revenue producing services. The path to managing the health status of communities at lower cost requires engagement and alignment of services outside of the acute care setting.
Key Take-Aways:
The future of the healthcare industry is uncertain. Care delivery is complex and multi-faceted with organizational gaps impeding the journey to designing and developing healthcare systems to meet ever increasing consumer expectations of value. The healthcare industry will continue to experience constant pressure to modify and change current care delivery systems to meet rising consumer expectations. Navigating the journey to coordinated care delivery across the full continuum of care requires strong vision for the future and a refined leadership philosophy.
This article provides a simplified approach to defining a compelling organizational vision. The need for a leadership style and organizational culture of performance excellence are outlined. Gaps in traditional organizational approach are also highlighted. The schematic below provides a roadmap for comprehensive improvement.
Future articles will provide additional detail related to how to lead the performance excellence journey to achieve an organizational vision of the future.
Next Step: Evaluate the company’s governance, leadership and management structure to identify opportunities for meaningful formal and informal engagement.
Performance Excellence Roadmap toward Value Based Care
Connect with us on LinkedIn and join our Active Network Program.
